Healthcare Burnout Crisis: Australia’s Silent Mental Health Battle
The Mental Health Cost of Burnout: What Australia’s Health Workers Are Saying
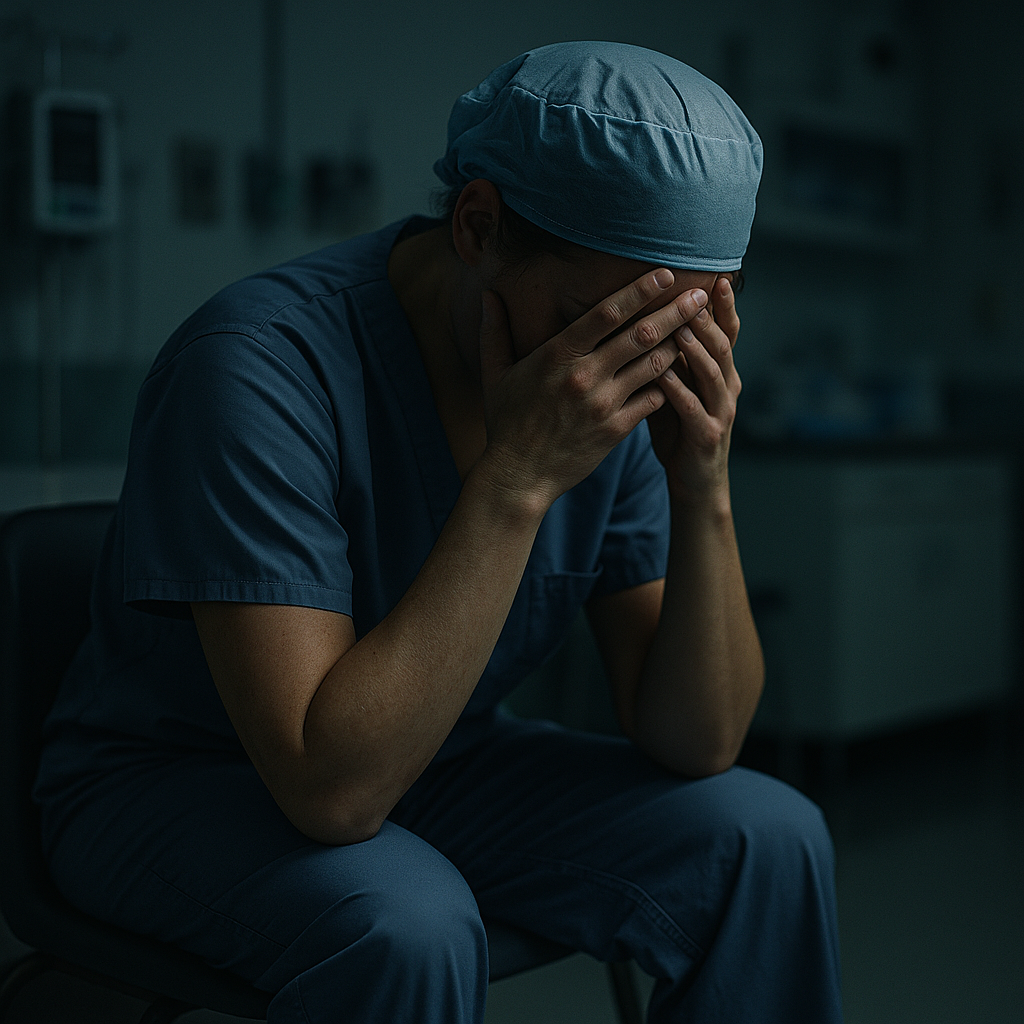
In the bustling corridors of Australia’s hospitals and healthcare facilities, a silent epidemic is spreading. It’s not a virus or a bacterial infection, but something equally insidious and potentially just as devastating: burnout. This pervasive issue is plaguing our healthcare system, affecting not just the well-being of individual health workers but also threatening the sustainability of the entire healthcare infrastructure.
As we delve into the heart of this crisis, we’ll explore the alarming statistics, hear from experts on the front lines, and uncover the profound impact burnout is having on both healthcare professionals and the patients they serve. More importantly, we’ll examine the crucial steps that must be taken to address this issue, ensuring the health and resilience of those who dedicate their lives to caring for others.
The State of Burnout in Australian Healthcare: A Growing Crisis
The numbers are stark and sobering. According to the latest data from Mental Health Australia’s annual survey, a staggering 84% of healthcare workers reported symptoms of burnout in 2022, a figure that has remained consistently high since the onset of the COVID-19 pandemic in 2020. This persistent trend indicates that burnout is not a temporary challenge but a chronic condition affecting the healthcare workforce.
Even more alarming is the broader context: 40% of Australian workers across all sectors report experiencing burnout, with healthcare professionals being particularly vulnerable. The impact on the healthcare system is profound, with 68% of staff absences related to burnout or mental health issues. These statistics paint a picture of a workforce under immense strain, struggling to cope with the demands placed upon them.
Looking ahead, the prognosis is equally concerning. Projections indicate a looming shortage of 100,000 nurses by 2025, a deficit that is expected to grow to 123,000 by 2030. This shortfall is heavily influenced by burnout and retention issues, creating a vicious cycle where staff shortages increase the burden on remaining workers, potentially exacerbating burnout rates further.
The Perfect Storm: Factors Contributing to Healthcare Burnout
The causes of burnout in healthcare are multifaceted and interconnected. At the systemic level, chronic staff shortages have led to increased workloads for existing staff. This high workload is compounded by the emotional strain inherent in patient care, particularly in high-stress environments such as emergency departments and intensive care units.
External stressors also play a significant role. The ongoing effects of the COVID-19 pandemic have left many healthcare workers feeling exhausted and overwhelmed. Additionally, socioeconomic pressures, including rising living costs and job insecurity, add to the mental burden carried by many in the healthcare sector.
Suhini Wijayasinghe, a workplace expert, highlighted in March 2025 the significant financial impact of burnout on businesses: “Burnout has a significant financial impact. Businesses suffer from absenteeism, lower productivity, and turnover when employees reach breaking point.” This observation underscores the far-reaching consequences of burnout, extending beyond individual well-being to affect organizational performance and sustainability.
The Ripple Effect: How Burnout Impacts Healthcare Delivery
The consequences of burnout extend far beyond the individual health worker. At an organizational level, increased staff turnover and absenteeism disrupt the continuity of care, potentially compromising patient safety and outcomes. The financial costs for employers are substantial, encompassing recruitment, onboarding, and lost productivity.
For individual health workers, the toll is both personal and professional. Mental health deterioration can lead to decreased job satisfaction, impaired decision-making, and in severe cases, exit from the profession altogether. This not only affects the individual’s career trajectory but also exacerbates the workforce shortages plaguing the healthcare sector.
The Grattan Institute, in a March 2022 report, emphasized the need for systemic workplace changes to address burnout effectively. The report noted that focusing solely on individual responsibility is insufficient and that meaningful change requires organizational-level interventions such as ensuring supervisor availability and protected time off.
Emerging Trends in Burnout Prevention: A Shift in Approach
As awareness of the burnout crisis grows, so too does the recognition that traditional approaches to managing workplace stress are inadequate. There is a growing emphasis on proactive, systemic solutions that address the root causes of burnout rather than merely treating its symptoms.
One significant trend is the adoption of technological solutions to support mental health. Digital platforms for anonymous mental health surveys and virtual counseling apps are becoming increasingly common, offering healthcare workers confidential access to support services.
Leadership development is another area of focus, with a growing emphasis on training healthcare leaders in emotional intelligence and burnout recognition. This approach aims to create a more supportive work environment where early signs of burnout can be identified and addressed before they escalate.
Sally McGrath, a workplace well-being expert, advocated in March 2025 for a fundamental shift in approach: “Organizations need to move from burnout firefighting to burnout blocking by embedding well-being into company culture.” This perspective highlights the importance of creating a workplace culture that prioritizes mental health and well-being as a core value rather than an afterthought.
Case Study: Express Healthcare Staffing’s Innovative Approach
A recent success story in burnout prevention comes from Express Healthcare Staffing, which implemented a comprehensive strategy to support their workers’ mental health. Their approach, detailed in a May 2025 blog post, included several key components:
- Flexible Scheduling: Recognizing the importance of work-life balance, the company introduced more flexible work options, including part-time roles and staggered shifts.
- Mental Health Check-ins: Regular “mental health huddles” were implemented, providing a safe space for staff to discuss their concerns and challenges.
- Leadership Training: Managers received specialized training in emotional intelligence and burnout recognition, equipping them to better support their teams.
- Cultural Shift: The company worked to foster a culture of open dialogue around mental health, reducing stigma and encouraging early intervention.
The results were significant: improved staff morale, lower turnover rates, and a general increase in job satisfaction among nursing teams. This case study demonstrates the potential impact of a comprehensive, organization-wide approach to burnout prevention.
How To: Supporting Healthcare Workers Against Burnout
For healthcare organizations looking to address burnout proactively, the following steps can serve as a starting point:
-
Implement Regular Mental Health Surveys
Use anonymous digital platforms to gauge the mental health of your workforce regularly. This data can help identify trends and areas of concern before they become critical. -
Provide Confidential Counseling and EAP Access
Ensure that all staff have easy access to confidential counseling services and Employee Assistance Programs. Consider offering virtual options to increase accessibility. -
Offer Flexible Scheduling Options
Where possible, introduce flexible work arrangements such as part-time roles, job sharing, or compressed work weeks. This can help staff better manage their work-life balance. -
Invest in Leadership Training
Equip managers and supervisors with the skills to recognize early signs of burnout and provide appropriate support. Focus on emotional intelligence and conflict resolution skills. -
Establish Recognition Programs
Regularly acknowledge and reward staff contributions. This can be through formal award programs or more informal peer-to-peer recognition systems.
By implementing these strategies, healthcare organizations can create a more supportive work environment that prioritizes mental health and well-being.
FAQs: Understanding and Addressing Healthcare Burnout
Q1: How does burnout differ from normal work stress?
A: While stress is a normal response to challenging situations, burnout is a state of physical, emotional, and mental exhaustion resulting from prolonged exposure to high levels of stress. Burnout is characterized by feelings of cynicism, detachment from work, and a sense of ineffectiveness.
Q2: Can burnout affect patient outcomes?
A: Yes, burnout can significantly impact patient care. Healthcare workers experiencing burnout may be more prone to errors, have reduced empathy, and provide lower quality care. This can lead to decreased patient satisfaction and potentially poorer health outcomes.
Q3: What role do healthcare leaders play in preventing burnout?
A: Leaders play a crucial role in burnout prevention. They set the tone for organizational culture, can implement supportive policies, and should model healthy work-life balance. Effective leaders also recognize early signs of burnout in their team and intervene appropriately.
Q4: How can healthcare workers recognize early signs of burnout?
A: Early signs of burnout may include feeling constantly tired, becoming easily irritated, losing enthusiasm for work, experiencing physical symptoms like headaches or muscle tension, and feeling disconnected from patients and colleagues.
Q5: Are there any legal protections for healthcare workers experiencing burnout?
A: While there are no specific legal protections for burnout, workplace health and safety laws require employers to provide a safe working environment, which includes managing psychological risks. Some workers may be eligible for stress leave or workers’ compensation if burnout leads to a diagnosed mental health condition.
Conclusion: A Call for Systemic Change
The burnout crisis in Australian healthcare is not just a challenge for individual workers—it’s a systemic issue that requires a coordinated, multifaceted response. As we’ve seen, the consequences of inaction are severe, threatening not only the well-being of healthcare professionals but also the quality and sustainability of our healthcare system.
The path forward requires a fundamental shift in how we approach workplace well-being in healthcare. It demands investment in mental health resources, leadership development, and cultural change. It calls for a reimagining of work structures to prioritize flexibility and work-life balance. Most importantly, it requires a collective commitment from healthcare organizations, policymakers, and society at large to value and protect the mental health of those who care for us in our times of greatest need.
As we look to the future, addressing burnout in healthcare must be seen not as an optional extra but as a critical component of healthcare policy and practice. Only by taking decisive action now can we hope to build a resilient, sustainable healthcare workforce capable of meeting the challenges of tomorrow.
The health of our nation depends on the health of our healthcare workers. It’s time we made their well-being our priority.
Author Name
Published on May 15, 2025