Nurse Burnout Crisis: 5 Essential Solutions for Mental Health
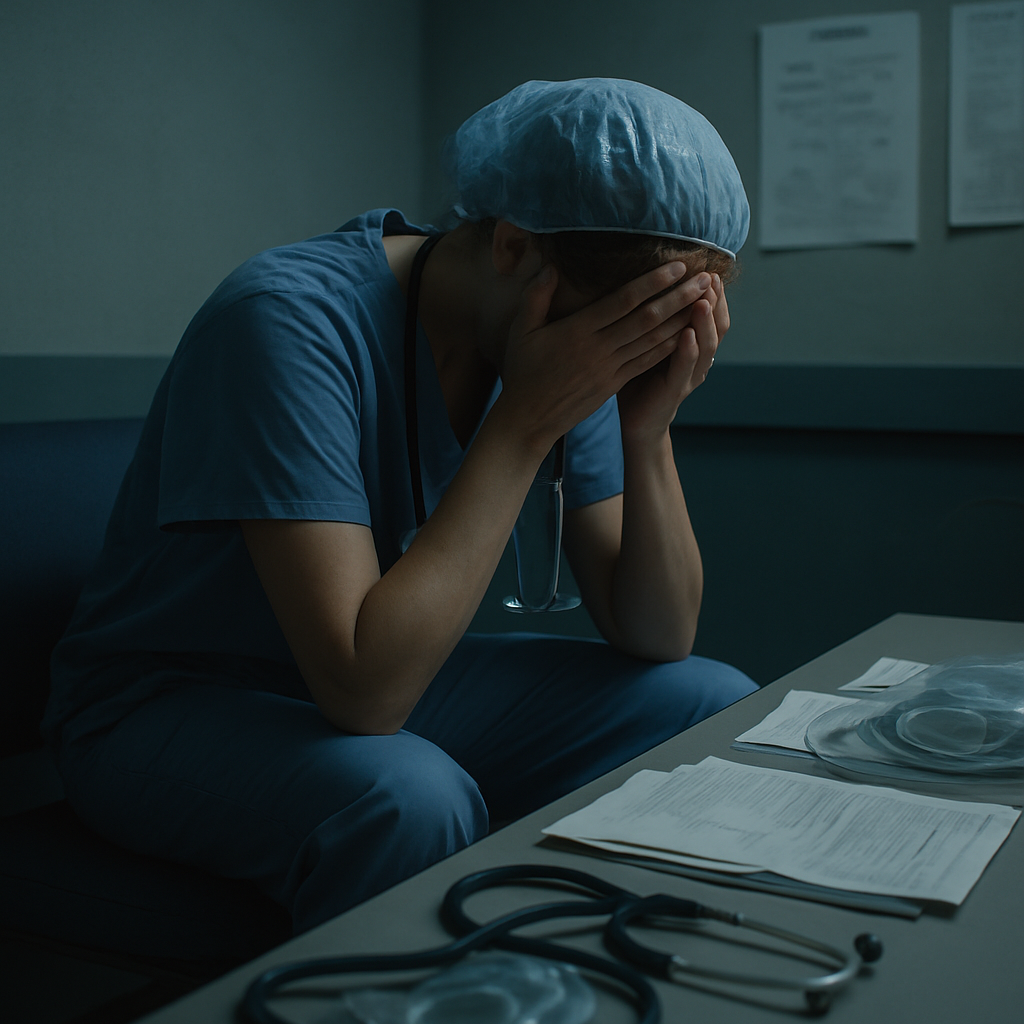
The Nurse Burnout Crisis: Causes, Impacts, and Solutions
In the world of healthcare, a silent epidemic is ravaging the very professionals we rely on to care for us in our most vulnerable moments. A startling 65% of nurses report high levels of stress and burnout, a statistic that should send shockwaves through the healthcare industry and society at large. This crisis of nurse burnout is not just a personal struggle for these dedicated professionals; it’s a looming threat to the sustainability of our entire healthcare system.
As we delve into this critical issue, we’ll explore the root causes of nurse burnout, its far-reaching impacts, and most importantly, the strategies that can help mitigate this growing problem. From the halls of bustling hospitals to the quiet corners where nurses catch their breath between shifts, the story of burnout is one that demands our attention and action.
Understanding Nurse Burnout: A Growing Crisis
Nurse burnout is more than just feeling tired after a long shift. It’s a state of physical, emotional, and mental exhaustion that occurs when nurses experience long-term stress in their job. This condition is characterized by a range of symptoms, including:
- Emotional exhaustion
- Depersonalization or cynicism towards patients
- Reduced sense of personal accomplishment
- Physical symptoms like headaches and insomnia
- Decreased job satisfaction and performance
Recent statistics paint a grim picture of the current state of nurse well-being:
- 61% of nurses worldwide report experiencing anxiety, depression, or burnout
- 57% of nurses feel exhausted every day at work
- Only 60% of nurses say they would choose nursing again if given the choice
These numbers are not just data points; they represent the lived experiences of countless nurses struggling to maintain their passion for caregiving in the face of overwhelming challenges.
Greg Coticchia, CEO of SE Healthcare, puts it bluntly: “Burnout isn’t just a personal struggle—it’s an institutional emergency.” This statement underscores the urgent need for systemic changes to address the burnout crisis.
The Perfect Storm: Causes of Nurse Burnout
The causes of nurse burnout are multifaceted and deeply rooted in the structure of our healthcare system. Understanding these factors is crucial for developing effective solutions.
1. Short Staffing and High Patient Ratios
One of the most significant contributors to nurse burnout is the issue of understaffing. A staggering 59% of nurses report being affected by short staffing and high patient ratios. This means that nurses are often responsible for more patients than they can safely and effectively care for, leading to:
- Increased stress and pressure to perform
- Inability to provide the desired level of care to each patient
- Higher risk of errors and oversights
- Lack of time for breaks or self-care during shifts
2. Inadequate Institutional Support
Many nurses feel that their institutions do not provide the support necessary to cope with the demands of their job. This lack of support can manifest in various ways:
- Insufficient resources for patient care
- Lack of recognition for their work and dedication
- Limited opportunities for professional development
- Inadequate policies to protect nurses from workplace violence or harassment
3. Lack of Mental Health Resources
Despite the high-stress nature of nursing, many workplaces fail to provide adequate mental health support. In fact, 24% of workplaces offer no mental health resources at all. This gap in support leaves nurses to cope with the emotional toll of their work on their own, often leading to burnout.
4. The Lingering Impact of COVID-19
The COVID-19 pandemic has exacerbated existing issues in nursing and created new challenges:
- Increased patient acuity and complexity of care
- Trauma from high patient mortality rates
- Constant fear of personal infection or transmitting the virus to loved ones
- Rapid changes in protocols and procedures leading to increased stress
The Ripple Effect: Impact of Nurse Burnout
The consequences of nurse burnout extend far beyond the individual nurses themselves, affecting patient care, healthcare institutions, and the broader healthcare system.
Patient Safety and Care Quality
Burnout directly impacts patient safety and the quality of care provided:
- Higher rates of medical errors
- Increased risk of hospital-acquired infections
- More frequent patient falls
- Lower patient satisfaction scores
When nurses are exhausted and overwhelmed, their ability to provide attentive, compassionate care is compromised, potentially leading to adverse outcomes for patients.
Healthcare Sustainability
The burnout crisis threatens the sustainability of our healthcare system in several ways:
- Workforce Exodus: Many nurses are leaving the profession altogether, exacerbating staffing shortages.
- Reduced Recruitment: The negative perception of nursing conditions may deter new entrants to the field.
- Financial Costs: High turnover rates and decreased productivity result in significant financial losses for healthcare institutions.
Mental Health Crisis Among Nurses
The personal toll of burnout on nurses’ mental health cannot be overstated:
- Increased rates of anxiety and depression
- Higher risk of substance abuse
- Elevated suicide rates among nurses compared to the general population
These mental health impacts not only affect the nurses themselves but also their families and communities.
Charting a Path Forward: Strategies to Combat Nurse Burnout
Addressing the nurse burnout crisis requires a multifaceted approach involving individual nurses, healthcare institutions, and systemic changes in the healthcare industry.
1. Institutional Support and Policy Changes
Healthcare organizations must take the lead in creating environments that support nurse well-being:
- Implement safe staffing ratios
- Provide comprehensive mental health resources and support
- Offer flexible scheduling options
- Create pathways for career advancement and professional development
2. Wellness Programs and Self-Care Initiatives
Promoting wellness and self-care can help nurses build resilience:
- Offer meditation and mindfulness programs
- Provide access to yoga and relaxation techniques
- Encourage regular breaks and time off
- Create spaces for rest and rejuvenation within healthcare facilities
3. Technology and Innovation
Leveraging technology can help alleviate some of the burdens on nurses:
- Implement efficient Electronic Health Record (EHR) systems
- Utilize AI and machine learning for routine tasks
- Explore telehealth options to manage patient load
- Adopt staffing management software to optimize schedules
4. Education and Training
Equipping nurses with the skills to manage stress and prevent burnout is crucial:
- Incorporate stress management and self-care into nursing education
- Provide ongoing training on coping strategies and resilience-building
- Offer leadership training to empower nurses in advocating for themselves
5. Systemic Healthcare Reform
Addressing nurse burnout requires broader changes in how we approach healthcare:
- Advocate for policies that prioritize nurse well-being
- Reform healthcare funding models to support better staffing ratios
- Promote a culture that values and respects nursing as a profession
Implementing a Personal Wellness Plan for Nurses
While systemic changes are crucial, individual nurses can take steps to protect their well-being:
- Assess Personal Stress Levels: Regularly check in with yourself to identify signs of burnout.
- Create a Self-Care Routine: Incorporate activities like meditation, exercise, or hobbies that bring joy and relaxation.
- Set Boundaries: Learn to say no and establish clear lines between work and personal life.
- Seek Support: Don’t hesitate to reach out to colleagues, mentors, or professional counselors for help.
- Practice Mindfulness: Use techniques like deep breathing or guided imagery during stressful moments at work.
- Prioritize Sleep and Nutrition: Ensure you’re getting adequate rest and maintaining a healthy diet.
- Engage in Continuous Learning: Pursue professional development opportunities to stay engaged and motivated in your career.
Frequently Asked Questions
How can nurses recognize early signs of burnout?
Early signs of burnout include feeling constantly tired, dreading going to work, becoming easily irritated, experiencing physical symptoms like headaches or insomnia, and feeling detached from patients or colleagues.
What role do hospital administrators play in preventing nurse burnout?
Hospital administrators are crucial in creating a supportive work environment. They can implement policies for safe staffing ratios, provide mental health resources, offer flexible scheduling, and foster a culture that values nurse well-being.
Are there any innovative technologies helping to reduce nurse workload?
Yes, several technologies are emerging to help reduce nurse workload, including AI-assisted patient monitoring, advanced EHR systems that streamline documentation, and staffing optimization software that ensures fair and efficient scheduling.
How can nurses advocate for better working conditions?
Nurses can advocate for better conditions by joining professional organizations, participating in workplace committees, communicating concerns to management, and supporting legislation that promotes nurse well-being and patient safety.
What are the long-term career implications of chronic burnout for nurses?
Chronic burnout can lead to decreased job satisfaction, reduced quality of patient care, increased risk of medical errors, and potentially leaving the nursing profession altogether. It can also have long-lasting effects on personal health and well-being.
Conclusion: A Call to Action
The nurse burnout crisis is not just a problem for nurses—it’s a threat to the entire healthcare system and, by extension, to all of us who rely on that system. As John A. Martins, president and CEO of Cross Country Healthcare, warns, “This year’s report is not just data — it’s a resounding cry for change. If we don’t act now, we risk losing an entire generation of dedicated professionals.”
Addressing this crisis requires a concerted effort from all stakeholders in healthcare:
- Nurses must prioritize their well-being and advocate for their needs.
- Healthcare institutions must implement supportive policies and create environments that foster nurse well-being.
- Policymakers must enact legislation that protects nurses and ensures safe working conditions.
- The public must recognize the value of nurses and support initiatives that promote their well-being.
By taking action now, we can work towards a future where nurses are empowered, supported, and able to provide the high-quality care that patients deserve. The health of our nurses is intrinsically linked to the health of our society. It’s time we gave them the care and support they so selflessly provide to others.